
A clinical warning system that uses wireless sensors to track the vital signs of at-risk patients is undergoing a feasibility study at Barnes-Jewish Hospital in St. Louis.
When the full system is operational sensors will take blood oxygenation and heart-rate readings from at-risk patients once or twice a minute. The data will be transmitted to a base station, where they will be combined with other data in the patient’s electronic medical record, such as lab test results.
The incoming vital signs and data in the medical record will be continually scrutinized by a machine-learning algorithm looking for signs of clinical deterioration. If any such signs are found, the system will call a nurse on a cell phone, alerting the nurse to check on the patient.
The idea is to create a virtual intensive care unit (ICU) where the patients aren’t wired to beeping machines and instead are free to move about as they please, say Chenyang Lu, PhD, a computer scientist at Washington University in St. Louis who was the principal investigator for the prototype-network trial.
The performance of the prototype network, which was installed at Barnes-Jewish Hospital from June 4, 2009, until Jan. 31, 2010, was described at the SenSys ’10 conference in Zurich, Switzerland. The feasibility study of the clinical warning system now under way at the hospital will be presented at the American Medical Informatics Association Annual Symposium this October.
The clinical warning system is part of a burgeoning new field variously called body sensor networks or wireless health that will change the future of medicine, Lu says.
Testbed in computer science department
The computer scientists thoroughly debugged the software and hardware for the warning system before the prototype was installed in the hospital.
A few years ago, anyone wandering around Jolley or Bryan halls, two buildings the WUSTL Department of Computer Science occupies on the Danforth Campus, might have noticed small green circuit boards the size of business cards poking out from between acoustic tiles in the ceiling. Occasionally, colored LEDs on the boards would blink on and off as the scientists experimented with their testbed.
Although the boards looked suspicious, they were only “motes,” wireless sensor nodes that were part of a testbed of 79 nodes that let the scientists test software and network protocols (rules for communication among nodes).
The motes contained sensors for light, temperature and humidity, says Lu, professor of computer science in the School of Engineering & Applied Science. “We had to assure our colleagues there were no microphones or cameras.”
Prototype in a step-down hospital unit
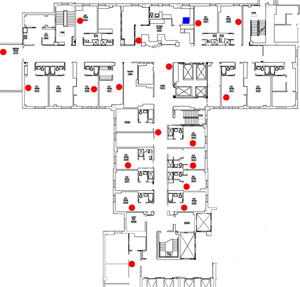
Once they worked out the kinks, the computer scientists installed a prototype network in a cardiac step-down unit at Barnes-Jewish Hospital.
Lu says he was pleased to find physicians and hospital administrators at Barnes-Jewish who were technology savvy and willing to let him install the prototype network. A step-down unit provides an intermediate level of care for patients who no longer require critical care but still need more care than is available on the general medical units.
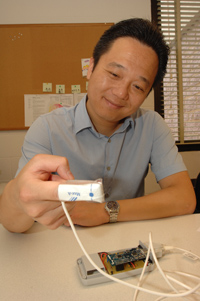
During the trial, consenting patients in the step-down unit wore a telemetry pouch around their necks and, on a finger, a pulse oximeter that measured heart rate and blood oxygenation. The sensor nodes transmitted the oximeter data through relay nodes to a base station, where it was saved in a database.
The prototype network was not integrated with clinical-warning algorithms. The data it reported was examined only after the fact to see whether it could have been used to correctly identify patients whose condition was deteriorating.
Clinical deterioration is a major concern in every hospital unit, says Thomas C. Bailey, MD, professor of medicine (infectious diseases) in the School of Medicine, who is working with Lu on the system. Of hospitalized patients, between 4 and 17 percent suffer an adverse event, such as a heart attack or respiratory arrest.
Most patients exhibit changes in their vital signs hours before an adverse event, sometimes as much as six hours before.
In ICUs, vital signs are continuously monitored by wired devices, but in the step-down units, they are often measured intermittently by the unit’s clinical staff. A wireless sensor network could monitor vital signs tens or hundreds of times more frequently.
Clever dodges
The computer scientists were focused on ensuring the network would always function and never go down. “To a technology guy, what’s most interesting is that the network reliably deliverd data to the endpoints, even if a few relays went silent,” Lu says.
The relay nodes were programmed as a self-organizing mesh network, meaning that if one node dropped out, data packets took another path to the base.
And indeed nodes did sometimes drop out, if only because the cleaning staff unplugged them to plug in floor cleaning machines.
The sensor and relay nodes both included a radio chip. The sensor nodes were battery powered, and the relay nodes were energized by USB-to-power adapters plugged into electrical outlets.
Because the scientists knew they couldn’t expect the nurses to take on extra duties like changing batteries, the sensor nodes hoarded power. A node turned on the radio only when it had a data packet to transmit, and turned off the radio as soon as a relay node acknowledged receipt of the packet.
When it first powered up, a sensor node “discovered” the relay nodes within its communication range and added them to a “neighbor table.” Then when it had data to transmit, it selected the neighbor at the start of the “lowest-cost” path to the base station for the first data hop.
If ambulatory patients wandered out of range of the relays in their tables, transmissions failed. The sensor counted transmission failures, and if there were too many, it flushed the neighbor table and “discovered” a new set of neighbors.
The surprises
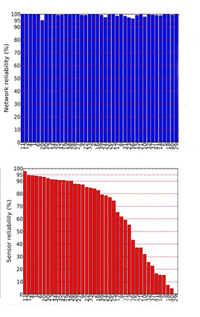
At the end of the trial, the computer scientists were pleased to learn the network was rock solid. Data were reliably received more than 99 percent of the time.
Sensing reliability was much lower, only 81 percent. Occasionally, a patient was wearing nail polish, which can block oximeter readings. Patient movement, such as gesturing, caused short bursts of failures, and some oximeters fell off or were removed, which led to long outages.
Because most of the failures occurred in short bursts, the scientists decided they could improve sensing reliability by over-sampling, that is, taking measurements at a rate higher than the one specified by clinical needs.
The best way to deal with disconnections, they decided, was to send an alarm if data failed to arrive for 10 or 15 minutes, a threshold that would result in an alarm rate low enough not to burden the nursing staff.
Lu says he was often asked why the team built a separate network instead of using the Wi-Fi network Barnes-Jewish recently installed for the convenience of their physicians and patients.
The mesh network uses less power, costs much less to install (because no wiring is needed), and can be deployed on demand, he says.
Did it work?
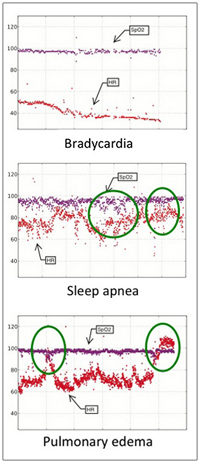
During the prototype trial, the condition of two patients deteriorated and a third patient was diagnosed with life-threatening sleep apnea.
Physicians looked at the vital-sign traces from the mesh network after the fact and confirmed that in all three cases the clinical deterioration could have been picked up from the traces.
The computer scientists also retroactively tested the ability of an algorithm that detects statistically significant changes in a series of measurements to identify these patients.
Knowing threshold values would have to be set low to avoid “alert fatigue,” a major problem in hospitals, they decided to integrate vital signs with data in the patients’ electronic medical records in the next-generation sensor network.
“Overall, the prototype trial showed that wireless sensor networks can successfully monitor vital signs to support real-time detection of clinical deterioration in patients,” Lu says.
To the future and beyond
The next-generation network is currently being developed and tested at the hospital. In the first tier of this two-tier system, a computer running a machine-learning algorithm calls nursing staff if new clinical data in an electronic medical record indicate a patient enrolled in the trial is at risk. The second-tier warning system, currently under development, will identify clinical deterioration based on both real-time data collected by the wireless sensors and regular clinical data in electronic medical records.
In addition to Bailey, who is the principal investigator for the clinical warning system trial, other faculty members on the team include Lu, Yixin Chen, PhD, associate professor of computer science in the School of Engineering & Applied Science, who developed the machine-learning algorithm; Marin H. Kollef, MD, professor of medicine (pulmonary diseases) and director of the medical intensive care unit; Scott Micek, PharmD, a clinical pharmacist at Barnes-Jewish and a faculty member at St. Louis College of Pharmacy; and Gruia-Catalin Roman, PhD, the former chair of the computer science department whose enthusiasm for distributed sensor networks helped inspire the project.
According to Lu, it won’t be long before any patient with a serious medical condition, such as diabetes or asthma, will wear a wireless medical device that will allow them to monitor their own vital signs on a smartphone that will also call relatives or doctors if serious problems arise.
The device for an asthma sufferer, for example, might keep track of respiration rate, air quality and pollen counts, among other features.
A frail patient might wear a wireless sensor with built-in accelerometers or gyroscopes that would monitor for falls.
The possibilities are endless and they all promise of better, more consistent care at lower cost, the primary objective of health care these days, Lu says.
This work is supported by a National Institutes of Health’s Clinical and Translational Science Award through the Washington University Institute of Clinical and Translational Sciences and the BJH Foundation.