Estrogen levels drop dramatically in menopause, a time when the risk of urinary tract infections increases significantly.
Researchers at Washington University School of Medicine in St. Louis have found new evidence in mice that the two phenomena are connected by more than just timing. If further research confirms these links, boosting estrogen levels may get a second look as an approach for reducing urinary infections in menopausal women.
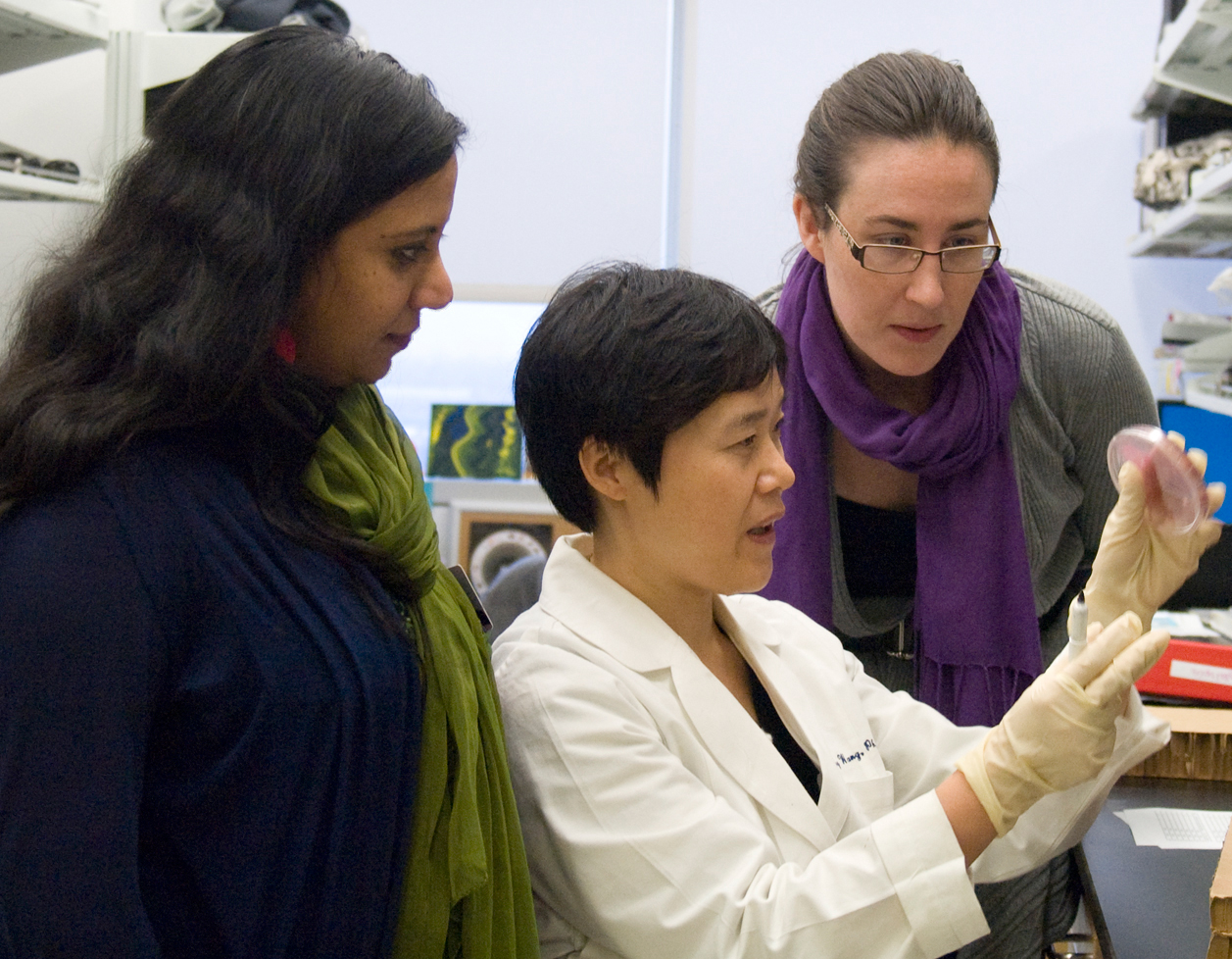
“Scientists tested estrogen as a treatment for post-menopausal women with urinary tract infections in the 1990s, but the results were either ambiguous or negative,” says senior author Indira Mysorekar, PhD, assistant professor of obstetrics and gynecology and of pathology and immunology. “With the mouse model of menopause that we’ve created, we can more completely understand how estrogen levels affect infection susceptibility, bladder health and the inflammatory response to infection. That should point the way to better treatment strategies.”
The findings appear online in Infection and Immunity.
Urinary infections are a significant cause of illness in many women throughout their lives and are particularly prevalent after menopause. The bacteria that cause these infections can spread to the kidney and bloodstream, with the potential for serious complications.
To simulate menopause in mice, scientists surgically remove their ovaries. Like menopausal women, the mice no longer make estrogen.
To rule out the possibility that the stress of surgery affects the risk of urinary tract infections, the researchers conducted the same surgery in other mice but put the ovaries back in, maintaining their ability to make estrogen.
When researchers gave both groups of mice urinary tract infections, the menopausal mice had higher levels of infectious bacteria in their urine. Most of the bacteria came from barrier cells, which line the interior of the bladder. These cells are the first to be infected by the bacteria.
“When the barrier cells are lost, they need to be replaced immediately,” Mysorekar says. “In the menopausal mice, we found that this replacement process was stopping short of completion. That left cells under barrier cells exposed, and they are much more vulnerable to infection.”
The menopausal mice had more bacterial reservoirs, which are pockets of infection that may provide a place for the bacteria to hide during antibiotic treatment. After treatment stops, the reservoirs can reseed the infection.
In earlier research, Mysorekar had identified an important regulator of the barrier cell repair process. In the new study, she showed that low estrogen levels disable this regulator.
The bladders of the menopausal mice also had higher levels of immune inflammatory compounds known as cytokines.
“The cytokines caused inflammation that left the bladder in bad shape,” Mysorekar says. “It’s possible that damage caused by inflammation increases the bacteria’s ability to break into bladder tissue and create reservoirs of infection.”
In the control mice, which had normal estrogen levels, cytokine levels and inflammatory damage were both significantly lower. When researchers gave the menopausal mice estrogen, their cytokine levels and inflammatory damage also decreased significantly, as did reservoirs of infectious bacteria.
Mysorekar notes that earlier clinical trials of estrogen’s usefulness against urinary infection evaluated the treatment’s success by tracking levels of bacteria in the urine. The researchers say their new results suggest that bacteria levels alone may not provide a complete picture of estrogen’s effectiveness against the infections.
“If we can find ways to look at other aspects of the infectious process in humans, we may find that estrogen is more helpful than we previously realized,” Mysorekar says. “We need to look for other indicators, such as cytokines in the urine, to more fully assess estrogen’s potential role in treatment.”
Wang C, Symington JW, Ma E, Cao B, Mysorekar IU. Estrogenic modulation of uropathogenic Escherichia coli pathogenesis in a murine menopause model. Infection and Immunity, March 2013.
Funding from the Center for Women’s Infectious Disease Research at Washington University (IUM) and the Multiplex Gene Analysis Core of the Siteman Cancer Center (supported in part by National Cancer Institute grant P30 CA91842) supported this research.
Washington University School of Medicine’s 2,100
employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine
is one of the leading medical research, teaching and patient care
institutions in the nation, currently ranked sixth in the nation by U.S.
News & World Report. Through its affiliations with Barnes-Jewish
and St. Louis Children’s hospitals, the School of Medicine is linked to
BJC HealthCare.