In laboratory tests on mice, researchers found that a medication often used to reduce toxic side effects of chemotherapy induced bone loss and helped tumors grow in bone. So the researchers at Washington University School of Medicine in St. Louis are recommending increased awareness of bone health during cancer treatments.
The medication studied is a growth factor commonly used to help cancer patients recover healthy blood counts after chemotherapy, which can destroy white blood cells. Low levels of white blood cells leave patients susceptible to infection.
“This growth factor encourages bone breakdown, and any therapy that decreases bone density could potentially enhance tumor growth in bone,” says senior author Katherine Weilbaecher, M.D., assistant professor of medicine and of cell biology and physiology. “But there are things that can be done to counteract this. Physicians should carefully monitor their cancer patient’s bone health with regular bone density scans (DEXA) and prescribe medications to prevent bone loss when needed. And patients should consume enough calcium and vitamin D and get sufficient exercise to maintain strong bones.”
Weilbaecher and her colleagues found that when they gave mice an eight-day course of the growth factor, called granulocyte colony-stimulating factor (G-CSF), the mice lost bone mass and experienced increased bone tumor growth when injected with cancer cells. Their study will appear in an upcoming issue of the journal Blood and is now available online.
G-CSF is known by the trade names Neupogen, Neulasta and Granocyte. Clinical use of G-CSF has recently increased because by speeding blood cell regrowth it allows patients to undergo more intensive chemotherapy regimens in which anticancer agents are given at more frequent intervals. Studies have suggested these dose-dense therapies could prolong survival in women with breast cancer.
“We are not at all advocating ending G-CSF use,” says Weilbaecher, an oncologist with the Siteman Cancer Center at Washington University School of Medicine and Barnes-Jewish Hospital. “G-CSF seems to have significant benefits for some cancer patients.”
Although G-CSF had a strong effect on bone metastasis in the experimental mice, early clinical trials in humans using G-CSF with chemotherapy have so far shown no adverse effects on survival and no increase in bone metastasis. In fact, breast-cancer patients undergoing dose-dense chemotherapy with G-CSF support tend to have a longer disease-free period than those getting standard dosing without G-CSF.
“It’s possible that women on G-CSF-supported chemotherapy could do even better if we paid more attention to skeletal health,” says lead author Angela Hirbe, an M.D./Ph.D. student in Weilbaecher’s lab. “Strengthening the skeleton would not only help prevent osteoporosis and fractures but also might give patients a survival advantage.”
In the laboratory mice studied, G-CSF increased the number and activity of bone cells called osteoclasts, which resorb bone material as part of the normal process of bone turnover. The resulting loss of bone density created a favorable environment for bone tumor growth.
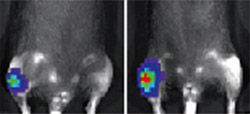
When the researchers injected melanoma or breast cancer cells into mice, those getting G-CSF developed a two-fold increase in tumor burden, a measure of the size and severity of tumors, compared to those that did not receive G-CSF.
Interestingly, mice treated with a bisphosphonate, an anti-osteoporosis agent that inhibits osteoclasts, were resistant to the effects of G-CSF on bone tumor growth. Weilbaecher is currently investigating bisphosphonates as a means to prevent tumor metastasis to bone in breast cancer patients.
“We used G-CSF as a tool to understand the implications for tumor growth when osteoclast activity is revved up,” Weilbaecher says. “But G-CSF isn’t unique in its effect. For example, antihormone therapies used to treat breast and prostate cancer also can decrease bone mineral density. We would like to see clinical trials instigated to study the effects of such cancer therapies on bone health and tumor metastasis.”
Hirbe AC, Uluçkan Ö, Morgan EA, Eagleton MC, Prior JL, Piwnica-Worms D, Trinkaus K, Apicelli A, Weilbaecher K. Granulocyte colony-stimulating factor enhances bone tumor growth in mice in an osteoclast-dependent manner. Blood Dec 27, 2006 (advance online publication).
Funding from the National Cancer Institute supported this research.
Washington University School of Medicine’s full-time and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked fourth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.
Siteman Cancer Center is the only NCI-designated Comprehensive Cancer Center within a 240-mile radius of St. Louis. Siteman Cancer Center is composed of the combined cancer research and treatment programs of Barnes-Jewish Hospital and Washington University School of Medicine.