Despite the abuse potential of opioid drugs, they have long been the best option for patients suffering from severe pain. The drugs interact with receptors on brain cells to tamp down the body’s pain response. But now, neuroscientists at Washington University School of Medicine in St. Louis have found a way to activate opioid receptors with light.
In a test tube, the scientists melded the light-sensing protein rhodopsin to key parts of opioid receptors to activate receptor pathways using light. They also influenced the behavior of mice by injecting the receptors into the brain, using light instead of drugs to stimulate a reward response.
Their findings are published online April 30 in the journal Neuron.
The eventual hope is to develop ways to use light to relieve pain, a line of discovery that also could lead to better pain-killing drugs with fewer side effects.
“It’s conceivable that with much more research we could develop ways to use light to relieve pain without a patient needing to take a pain-killing drug with side effects,” said first author Edward R. Siuda, a graduate student in the laboratory of Michael R. Bruchas, PhD, an assistant professor of anesthesiology and of neurobiology.
But before that’s possible, the researchers are attempting to learn the most effective ways to activate and deactivate the opioid receptor’s pathways in brain cells. Bruchas, the study’s principal investigator, explained that working with light rather than pain-killing drugs makes it much easier to understand how the receptors function within the complex array of cells and circuits in the brain and spinal cord.
“It’s been difficult to determine exactly how opioid receptors work because they have multiple functions in the body,” Bruchas explained. “These receptors interact with pain-killing drugs called opiates, but they also are involved in breathing, are found in the gastrointestinal tract and play a role in the reward response.”
So the researchers sought a way to limit opioid receptors to performing a single task at a time, and it turned out to be almost as easy as flipping on a light switch, according to Bruchas, Siuda and their collaborators, including co-first author Bryan A. Copits, PhD, a postdoctoral research scholar in the laboratory of Robert W. Gereau, IV, PhD, the Dr. Seymour and Rose T. Brown Professor of Anesthesiology.
By combining the rhodopsin protein, which senses light in the eye’s retina, with a specific type of opioid receptor called a Mu opioid receptor, the researchers were able to build a receptor that responds to light in exactly the same way that standard opioid receptors respond to pain-killing drugs.

When an opioid receptor is exposed to a pain-killing drug, it initiates activity in specific chemical pathways in the brain and spinal cord. And when the researchers shone light on the receptors that contained rhodopsin, the same cellular pathways were activated.
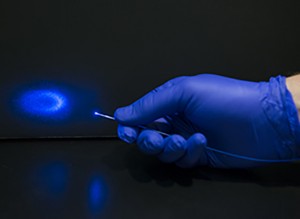
In a test tube and in cells, Siuda exposed the receptors to light and then watched as they released the same chemicals that standard opioid receptors release. Then, in mice, the researchers implanted a light-emitting diode (LED) device the size of a human hair into a brain region linked to the reward response. They injected the light-sensing receptors they had genetically manufactured into the same brain region. Neurons in that part of the brain release chemicals such as dopamine that create feelings of euphoria.
In decades of past opioid studies, researchers have observed mice and rats press a lever to receive a dose of morphine, for example. The morphine would activate opioid receptors and the release of dopamine, and the animals would enjoy the response and press the lever again to continue feeling that reward sensation. This is one of the reasons opiates are so often abused in patients being treated for pain — people like the way the drugs make them feel as much as the pain relief they provide — and rates of abuse have skyrocketed over the past 10 years.
Working to deliver a similar reward sensation using light, the researchers put the mice into an enclosed chamber. In one part of the chamber, the lighted laser fiber-optic device stimulated the release of dopamine in the brain. When the animals left that part of the chamber, the light in the brain turned off. Soon after, the mice returned to the part of the chamber that activated the fiber-optic device so that the brain could receive more light stimulation.
“By activating the receptors with light, we are presumably causing the brain to release more dopamine,” Bruchas explained. “Rather than a drug such as morphine activating an opioid receptor, the light provides the reward.”
The researchers were able to vary the animals’ response depending on the amount and type of light emitted by the LED. Different colors of light, longer and shorter exposure to light, and whether the light pulsed or was constant all produced slightly different effects.
When a person takes an opioid drug such as Vicodin or OxyContin to relieve pain, such drugs interact with receptors in the brain to blunt pain sensations. But over time, patients develop tolerance and sometimes addiction. Opioids also can dramatically slow a person’s breathing, too, and typically cause constipation.
In theory, receptors tuned to light may not present the same danger. Siuda said it someday may be possible to activate, or deactivate, nerve cells without affecting any of the other receptors that pain-killing drugs trigger, although achieving that goal will be difficult.
Bruchas’ team is planning future studies that will use these receptors to test ways to control the brain cells that mediate pain and reward behavior with light rather than drugs.
The research was supported by a EUREKA award from the National Institute on Drug Abuse, the National Institute of Mental Health and the National Institute of General Medical Sciences of the National Institutes of Health (NIH), grant numbers R01 DA037152, F31 MH101956, K99 DA038725, TR32 GM108539 and NSTR01 NS081707. Additional funding from a W.M. Keck Fellowship in Molecular Medicine; and the Howard Hughes Medical Institute.
Siuda ER, Copits BA, Schmidt MJ, Baird MA, Al-Hasani R, Planer WJ, Funderburk SC, McCall JG, Gereau RW, Bruchas M. Spatiotemporal control of opioid signaling and behavior. Neuron, published online April 30, 2015.
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient-care institutions in the nation, currently ranked sixth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.