Adults diagnosed with ulcerative colitis after age 50 are more likely to achieve remission from their symptoms than patients diagnosed at younger ages, even when those patients receive similar treatments, according to research at Washington University School of Medicine in St. Louis.
The study, published in the August issue of Clinical Gastroenterology and Hepatology, is the first to look at patients whose colitis was treated with modern medications, from the relatively mild, maintenance drugs known as 5-aminosalicylates (5-ASAs) to immunosuppressive therapies such as steroids and the drug infliximab, which targets specific proteins in the body’s immune system to help control inflammation.
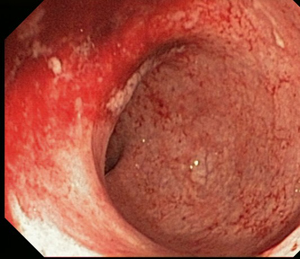
Nearly 1 million U.S. adults have ulcerative colitis. The related Crohn’s disease can affect any part of the gastrointestinal tract, but ulcerative colitis patients have inflammation only in the lining of the large intestine or colon. The condition often causes diarrhea, bloody stool, weight loss and fever. In severe cases, some patients need surgery to remove the colon.
“At the start of the study, our early- and late-onset patient groups were about equal in terms of the severity of their symptoms,” according to lead investigator Matthew A. Ciorba, MD, assistant professor of medicine at Washington University. “However, after a year of treatment, those who had developed colitis later in life had better outcomes. More of them were in clinical remission at one year, compared to those diagnosed when they were younger.”
The study involved 295 people treated at the inflammatory bowel disease clinics at the School of Medicine over a seven-year period from 2001-08. After treatment, 64 percent of patients diagnosed after the age of 50 were in remission, compared to 49 percent of those who developed colitis at younger ages. Patients in remission no longer have clinical symptoms of colitis, but many may still have inflammation and may need to continue treatment with 5-ASA drugs but are able to discontinue steroids.
Ciorba says those diagnosed early in life were more likely to have family members with inflammatory bowel disease and that genetic influences may play a larger role in their disease. More than one in five study patients under age 30 had a family history of inflammatory bowel disease.
“The age at which patients are affected tends to split into two specific waves,” Ciorba says. “In the clinic, we see a number of patients who get the disease from their late teens to their mid 20s. Then there’s a second peak of patients who aren’t affected until after the age of 50.”
The researchers suspect that later-onset disease is related to changes in the aging immune system and to environmental influences such as smoking. Nearly 52 percent in the late-onset group were former smokers, compared with only 13.5 percent of the younger patients. Smoking is a well-known risk factor for colitis.
“We know from research by other investigators that as people age their immune systems tend to quiet down, and the results from our study may reflect that finding,” Ciorba says. “Ulcerative colitis is driven by an over-active immune response in the gut, so it makes sense that people whose immune systems are less active might have better outcomes. Conversely, younger patients are more likely to have robust inflammatory responses, so their disease is harder to quiet down.”
Both younger and older patients received the same treatments, mainly 5-ASAs and steroids. About 63 percent of early-onset patients and 68 percent of late-onset patients received either oral or intravenous steroids within the first year of treatment.
“Steroids have long been used as a therapy, but they are a ‘dual-edged sword’ in many cases,” he says. “They improve symptoms, but we are not sure that they actually promote healing in the colon. The good news is that for many patients, regardless of their age at disease onset, aggressive, early therapy is related to relatively high remission rates.”
Ciorba’s team says more research is needed into the environmental and genetic factors that differentiate late- versus early-onset disease. That work could help determine whether older or younger patients may respond better to different therapeutic combinations or newer investigative therapies.
Ha CY, Newberry RD, Stone CD, Ciorba MA, Patients with late adult onset ulcerative colitis have better outcomes than those with early onset disease. Clinical Gastroenterology and Hepatology, August 2010; DOI: 10.1016/j.cgh.2010.03.022
The study was funded by grants from the National Institutes of Health and by a career development award given to Matthew Ciorba from the Crohn’s and Colitis Foundation of America.
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked fourth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.