A provocative study links prolonged episodes of sepsis — a life-threatening infection and leading cause of death in hospitals — to the reactivation of otherwise dormant viruses in the body.
In healthy people, such latent viruses are kept in check by the immune system. But a study by a team at Washington University School of Medicine in St. Louis provides strong evidence that when sepsis lingers for more than a few days, which is common, viruses re-emerge and enter the bloodstream, signaling that the immune system has become suppressed. This state of immune suppression may leave patients unable to fight off secondary infections, such as pneumonia associated with being on a ventilator.
The research, published June 11 in PLOS One, suggests that drugs that “rev up” the immune system could be incorporated into the treatment of prolonged sepsis.
“A controversy has existed over whether patients with sepsis progress to a state of immune suppression,” said co-senior author Gregory Storch, MD, a virologist and chief of the Division of Pediatric Infectious Diseases. “The finding that critically ill patients with sepsis have a number of different viruses circulating in the bloodstream is compelling evidence they are immune-suppressed and dramatically could alter therapy for sepsis.”
Surprisingly, the researchers detected levels of viruses in sepsis patients that were on par with those seen in patients who have had organ transplants and are taking immune-suppression drugs to prevent rejection.
“This is an indicator of the degree of immune suppression in septic patients, and it tells us they are highly immune-suppressed,” explained senior author Richard S. Hotchkiss, MD, professor of anesthesiology.
More than 200,000 patients in the United States die annually of sepsis. The condition develops when the body mounts a massive immune response to infection, triggering excessive inflammation that can lead quickly to organ failure. While some patients die soon after the condition develops, most sepsis deaths occur four or more days after onset.
“We’ve gotten much better at getting sepsis patients through the initial phase,” said Hotchkiss, who also is a professor of medicine and of surgery. “But too many patients die several weeks or months after sepsis sets in, primarily of secondary infections.”
Earlier research at Washington University and other institutions has hinted that lingering sepsis may be linked to immune suppression. But a lack of compelling evidence has kept the debate going.
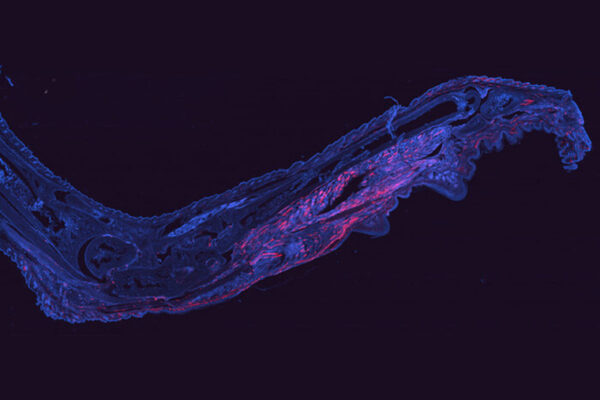
For the current study, first authors Andrew Walton and Jared Muenzer, MD, used polymerase chain reaction (PCR) testing to detect a range of viruses in blood and urine samples from 560 critically ill patients with sepsis, who were treated in the surgical and medical intensive care units at Barnes-Jewish Hospital. As a comparison, they performed the same test on 161 critically ill patients in the hospital who did not have sepsis and 164 healthy patients who were having outpatient surgery.
“We were looking for viruses that people are commonly exposed to early in life and that persist in the body in a latent form that doesn’t cause sickness,” said Storch, the Ruth L. Siteman Professor of Pediatrics. “No one had really looked at this in a comprehensive fashion before. These viruses have the potential to reactivate if the immune system is suppressed.”
Patients with lingering sepsis had markedly higher levels of viruses detectable in the blood, compared with the healthy controls and critically ill patients without sepsis. Among the sepsis patients, for example, the researchers found that 53 percent had Epstein-Barr virus, 24 percent had cytomegalovirus, 14 percent had herpes-simplex virus, and 10 percent had human herpes simplex virus-7.
These viruses generally don’t lead to significant illness in people who are healthy but can cause problems in patients who are immune-suppressed.
The researchers noted that 43 percent of patients with sepsis had two or more viruses detected in their blood or urine during their hospital stays. However, this finding may underestimate the frequency of viral infections because some of these patients were not tested for all viruses. In a subgroup of 209 sepsis patients tested for all viruses, 54 percent were positive for two or more.
Additionally, the researchers found that septic patients with higher levels of viruses detected in their blood were more likely than critically ill patients without sepsis to have more severe illnesses, secondary fungal and bacterial infections, and longer stays in the intensive care unit.
Also, septic patients with evidence of cytomegalovirus in plasma, a component of blood, had significantly higher 90-day death rates than septic patients who tested negative for the virus, although it is not clear whether the cytomegalovirus contributed to the additional deaths.
“We stumbled onto more viruses than we expected, and we don’t know yet whether some of these viruses are causing problems in their own right,” Storch said. “We think this paper will stimulate others to carry out further investigations of the role of latent viruses in sepsis.”
A further direction for researchers is to determine whether PCR testing for a panel of latent viruses could be used as a readout of the state of a person’s immunity. If this is the case, doctors could perform PCR testing in patients with cancer, autoimmune diseases and infections and use results to guide treatments.
The findings also open the door to new ways of treating sepsis. Over the years, a number of treatments have been evaluated to treat sepsis, but none has worked well. The new research indicates that, in addition to using powerful antibiotics to fight off infections in patients with sepsis, immunotherapy drugs that boost the immune system may be an effective therapy. The Washington University team is planning several clinical trials of such drugs in sepsis patients in the near future.
The research was funded by the National Institutes of Health (NIH), grants GM044118 and GM098391.
Walton AH, Muenzer JT, Rasche D, Boomer JS, Sato B, Brownstein BH, Pachot A, Brooks TL, Deych E, Shannon WD, Green JM, Storch GA and Hotchkiss, RS. Reactivation of multiple viruses in patients with sepsis. PLOS One. June 11, 2014.
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient-care institutions in the nation, currently ranked sixth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.